Begin with a low dose, typically 5-10mg daily, under strict medical supervision. Your doctor will adjust this based on your specific condition and response. Remember, Prednisone isn’t a long-term solution for arthritis.
Dosage adjustments are common. Expect gradual increases if needed, but always within your doctor’s prescribed range. Rapid changes can lead to negative side effects. Closely monitor your body’s reaction and promptly report any concerns.
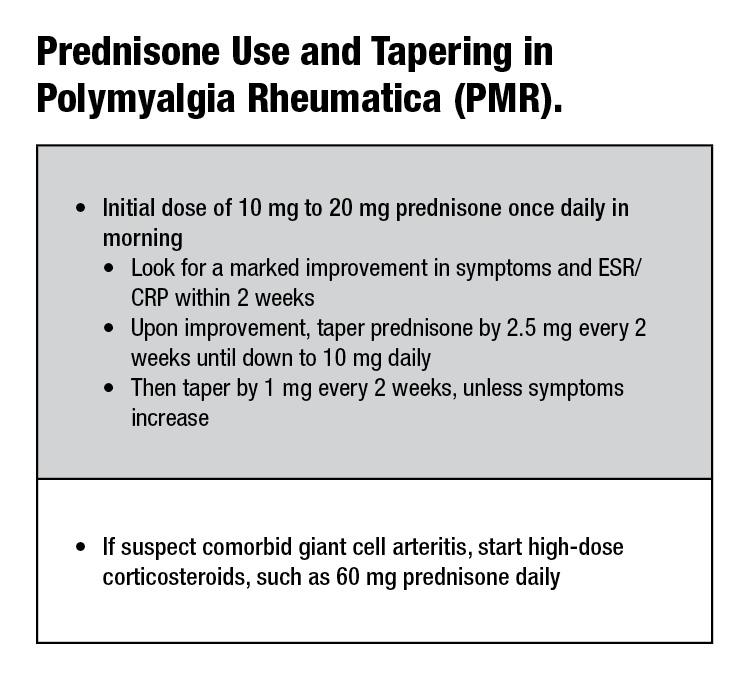
Tapering off Prednisone is crucial. Sudden cessation can trigger withdrawal symptoms. Your rheumatologist will design a gradual reduction plan, ensuring a smoother transition. This usually involves a slow, step-wise decrease over weeks or months.
Side effects are possible. Common ones include weight gain, increased appetite, mood changes, and insomnia. Less frequent but more serious side effects require immediate medical attention. Open communication with your healthcare provider is key to managing these.
Always consult your doctor or rheumatologist before changing your Prednisone dosage. They possess the expertise to tailor a treatment plan to your individual needs and health history. Self-adjusting can be harmful.
- Prednisone Dosage for Arthritis: A Comprehensive Guide
- Initial Dosage and Tapering
- Maintenance Dosage
- Specific Arthritis Types
- Side Effects and Monitoring
- Alternative and Complementary Therapies
- Discontinuing Prednisone
- Understanding Prednisone’s Role in Arthritis Treatment
- Common Arthritis Types Treated with Prednisone
- Standard Prednisone Dosage Ranges for Arthritis
- Factors Influencing Prednisone Dosage Adjustments
- Potential Side Effects of Prednisone and Mitigation Strategies
- Common Side Effects and Management
- Less Common but Serious Side Effects
- Tapering Off Prednisone: A Gradual Approach
- Monitoring Your Body’s Response
- Potential Side Effects During Tapering
- Sample Tapering Schedule (Consult your doctor!)
- Maintaining Communication
- Monitoring Progress and Communicating with Your Doctor
- Tracking Side Effects
- Communicating Effectively
- Alternative Treatments and Complementary Therapies
- Dietary Changes
- Mind-Body Techniques
Prednisone Dosage for Arthritis: A Comprehensive Guide
Prednisone dosages for arthritis vary greatly depending on the type of arthritis, severity of symptoms, and individual patient response. Your doctor will determine the appropriate dose and treatment duration. Generally, treatment begins with a higher dose to quickly reduce inflammation, followed by a gradual tapering to minimize side effects. Typical starting dosages range from 5 to 60 mg daily, though higher initial doses might be used in severe cases.
Initial Dosage and Tapering
A rheumatologist will likely prescribe a higher initial dose (e.g., 40-60 mg daily) for a short period to control acute inflammation. This is then reduced gradually over several weeks or months. The tapering schedule is personalized and depends on your response to treatment and the presence of side effects. Rapid tapering is generally avoided to prevent symptom flare-ups.
Maintenance Dosage
Once symptoms are under control, the goal is to maintain the lowest effective dose. This could range from 5 to 10 mg daily, or even less. Long-term use requires careful monitoring for side effects.
Specific Arthritis Types
Dosage adjustments may be necessary depending on the type of arthritis. For instance, patients with rheumatoid arthritis may require higher doses initially compared to those with osteoarthritis. Your physician will tailor the treatment to your specific condition.
Side Effects and Monitoring
Prednisone has potential side effects, including increased blood sugar, weight gain, high blood pressure, and bone thinning. Regular monitoring of blood pressure, blood sugar, and bone density is crucial, particularly during long-term use. Report any concerning symptoms to your doctor immediately.
Alternative and Complementary Therapies
Prednisone often works in conjunction with other disease-modifying antirheumatic drugs (DMARDs) or biologics. Your doctor will determine the most appropriate treatment plan for you, potentially incorporating non-pharmacological interventions like physical therapy and exercise.
Discontinuing Prednisone
Never stop taking Prednisone abruptly without consulting your physician. Sudden cessation can lead to a severe flare-up of symptoms. Always follow your doctor’s instructions regarding dosage reduction to ensure a safe and effective transition.
Understanding Prednisone’s Role in Arthritis Treatment
Prednisone, a corticosteroid, doesn’t cure arthritis, but it powerfully reduces inflammation and pain, offering significant relief. Doctors prescribe it to manage flare-ups, especially in severe cases. Its anti-inflammatory action targets the underlying cause of many arthritis symptoms.
Here’s what you should know:
- Pain Relief: Prednisone rapidly reduces pain and stiffness, improving mobility and quality of life.
- Inflammation Reduction: It directly targets the inflammatory process characteristic of arthritis, lessening joint swelling and tenderness.
- Disease Modification: While not a disease-modifying antirheumatic drug (DMARD), Prednisone can slow disease progression in some cases when used in conjunction with DMARDs.
However, long-term use carries potential side effects. Therefore, doctors typically prescribe Prednisone for short periods or in carefully managed low doses. Strategies include:
- Pulse Therapy: High doses for a short time, followed by tapering down to minimize side effects.
- Low-dose Maintenance: A small daily dose to manage persistent symptoms while mitigating long-term risks.
- Alternating-day Therapy: Taking the medication every other day to reduce side effects.
Potential side effects include weight gain, increased blood sugar, increased risk of infection, and thinning of bones. Regular monitoring by your doctor is crucial to manage these risks. Open communication with your doctor about your symptoms and any side effects is vital for safe and effective treatment. Always follow your doctor’s prescribed dosage and schedule.
Remember, Prednisone is a powerful medication. Never start or stop taking it without consulting your doctor. They’ll help you determine the best course of action based on your specific needs and health condition.
Common Arthritis Types Treated with Prednisone
Prednisone, a corticosteroid, effectively manages inflammation in several arthritis types. Its use is often short-term, due to potential side effects. Let’s explore some common conditions:
- Rheumatoid Arthritis (RA): Prednisone quickly reduces RA symptoms like joint swelling and pain. Doctors often prescribe it initially, alongside disease-modifying antirheumatic drugs (DMARDs), for faster symptom relief. Dosage varies significantly depending on the severity of the disease and the patient’s response. Always follow your doctor’s instructions.
- Osteoarthritis (OA): While not primarily treated with prednisone, it can offer temporary pain relief in severe OA flare-ups. Doctors usually prefer other treatments, such as pain relievers and physical therapy, as long-term prednisone use carries risks in OA.
- Psoriatic Arthritis (PsA): Prednisone is sometimes used for PsA to manage inflammation and pain during acute flares. However, similar to OA, other therapies are usually preferred for long-term management. The goal is to control symptoms and prevent joint damage.
- Gout: In acute gout attacks, prednisone can reduce inflammation and pain. However, it does not treat the underlying cause, hyperuricemia. Colchicine or other medications are typically preferred for gout management.
- Lupus (Systemic Lupus Erythematosus): Prednisone helps manage lupus-related joint inflammation. It’s often part of a broader treatment strategy to control the autoimmune response. Long-term use requires careful monitoring due to potential side effects.
Remember: Prednisone is a powerful medication. Your doctor will determine the appropriate dosage and duration based on your specific condition and overall health. Discuss potential side effects and any concerns with your physician before starting treatment.
- Always follow your doctor’s instructions precisely.
- Report any side effects immediately.
- Never adjust your dosage without consulting your physician.
Standard Prednisone Dosage Ranges for Arthritis
Prednisone dosages for arthritis vary greatly depending on the type of arthritis, severity of symptoms, and individual patient response. Your doctor will determine the appropriate dosage for you. However, typical starting dosages range from 5 to 60 milligrams per day.
Initial treatment often involves higher doses, sometimes exceeding 60 mg daily, to quickly control inflammation. This high-dose therapy is usually short-term, lasting only a few days or weeks.
Maintaining remission usually requires lower doses. Once symptoms improve, your doctor will gradually reduce your dosage to the lowest effective level. This is done to minimize side effects while managing arthritis symptoms.
Typical maintenance dosages often fall between 5 and 10 milligrams daily. However, some individuals may require higher maintenance dosages, while others may respond well to even lower doses.
Dosage adjustments are common. Your doctor may adjust your dosage based on your response to treatment and the presence of side effects. Regular monitoring is critical for optimal management of your condition and minimizing potential adverse effects.
Remember: This information is for general knowledge only and does not substitute for professional medical advice. Always consult with your rheumatologist or physician before starting or changing any medication, including Prednisone.
Factors Influencing Prednisone Dosage Adjustments
Your doctor will personalize your prednisone dosage based on several key factors. Severity of your arthritis symptoms significantly impacts the initial dose. More intense pain and inflammation generally necessitate a higher starting dose.
Your overall health plays a crucial role. Pre-existing conditions, such as diabetes or heart problems, may require a lower prednisone dose or careful monitoring. Liver and kidney function also influence how your body processes the medication. Your doctor will adjust the dose accordingly.
Response to treatment is another critical factor. If your symptoms improve significantly, your doctor might gradually reduce your dose. Conversely, if your symptoms persist or worsen, they may increase the dose or explore alternative treatment options.
Age is also a consideration. Older adults often require lower doses due to increased risk of side effects. Body weight also influences how much prednisone your body absorbs and processes; larger individuals may require higher doses.
Other medications you’re taking can interact with prednisone, potentially influencing its effectiveness and side effects. Always inform your doctor of all medications and supplements you’re using.
Regular monitoring of your condition is necessary. Blood tests might be used to assess your response and monitor for potential side effects. Based on these results, your doctor will fine-tune your dosage to optimize therapeutic benefit and minimize adverse effects.
Potential Side Effects of Prednisone and Mitigation Strategies
Prednisone, while effective for arthritis pain relief, carries potential side effects. Understanding these and employing mitigation strategies is key to managing treatment effectively.
Common Side Effects and Management
Weight gain is frequent. Counter this with a balanced diet and regular exercise. Increased appetite is also common; mindful eating helps. Mood changes, including irritability and anxiety, can occur. Regular physical activity and stress-reduction techniques like yoga or meditation can provide support. Fluid retention can lead to swelling; limiting sodium intake aids this. Increased blood sugar levels are possible, particularly in those with diabetes. Careful blood sugar monitoring and adjustments to diabetes medication, if needed, are critical.
Less Common but Serious Side Effects
Osteoporosis, a weakening of bones, is a potential risk. Regular weight-bearing exercise and sufficient calcium and Vitamin D intake help prevent this. Increased risk of infection requires vigilance in hygiene and prompt medical attention for any signs of infection. Glaucoma and cataracts can develop; regular eye exams are necessary. High blood pressure is possible. Regular blood pressure monitoring and dietary modifications are beneficial.
Always discuss any concerns or new symptoms with your doctor. Early intervention is essential for managing potential complications. Your doctor can adjust your dosage or prescribe additional medications to minimize side effects. Open communication is crucial for successful Prednisone therapy.
Tapering Off Prednisone: A Gradual Approach
Never stop Prednisone abruptly. Always reduce your dosage gradually under your doctor’s supervision. Rapid withdrawal can trigger serious side effects.
Your doctor will create a personalized tapering schedule, usually involving small, regular reductions in your daily dose. This schedule is tailored to your individual needs and medical history. A typical schedule might involve decreasing the dose by 2.5mg every few days or weeks. For example, if you’re on 20mg, your doctor might prescribe 17.5mg for a week, then 15mg, and so on.
Monitoring Your Body’s Response
Closely monitor your symptoms throughout the tapering process. Report any new or worsening symptoms, such as fatigue, joint pain, or muscle weakness, to your doctor immediately. These changes may indicate the need to adjust the tapering schedule.
Potential Side Effects During Tapering
You may experience some side effects during tapering, including fatigue, joint pain, and mood changes. These side effects are generally temporary and manageable. Your doctor can help mitigate these issues.
Sample Tapering Schedule (Consult your doctor!)
| Week | Daily Dose (mg) |
|---|---|
| 1 | 20 |
| 2 | 17.5 |
| 3 | 15 |
| 4 | 12.5 |
| 5 | 10 |
| 6 | 7.5 |
| 7 | 5 |
| 8 | 2.5 |
| 9 | 0 |
This is just a sample schedule. Your doctor will determine the most appropriate tapering plan for you, depending on factors like your initial dosage, duration of treatment, and overall health.
Maintaining Communication
Regular communication with your doctor is vital throughout the tapering process. Schedule follow-up appointments to discuss your progress and make any necessary adjustments to your medication plan.
Monitoring Progress and Communicating with Your Doctor
Keep a detailed record of your symptoms. Note pain levels (using a scale of 1-10), stiffness, swelling, and any other relevant information daily. This detailed log helps your doctor track your response to Prednisone effectively.
Schedule regular check-ups. Your doctor will want to see you at least monthly, potentially more frequently initially, to monitor your blood pressure, blood sugar, and other potential side effects. Be prepared to discuss your progress openly during these appointments.
Tracking Side Effects
Prednisone can cause various side effects, including weight gain, increased blood pressure, and mood changes. Report any new or worsening symptoms immediately. Don’t hesitate to contact your doctor if you experience anything concerning, even if it seems minor.
Communicating Effectively
Before your appointment, prepare a list of questions. This ensures you address all your concerns and understand your treatment plan fully. Don’t be afraid to ask for clarification if anything is unclear. Active participation in your care yields the best results.
Maintain open communication between appointments. If your symptoms change significantly or you experience troubling side effects, contact your doctor’s office without delay. Prompt communication can prevent complications and ensure the most effective management of your arthritis.
Alternative Treatments and Complementary Therapies
Consider adding regular low-impact exercise like swimming or walking to your routine. Aim for at least 30 minutes most days of the week. This helps improve joint mobility and overall strength, potentially reducing pain and stiffness.
Dietary Changes
A balanced diet rich in anti-inflammatory foods such as fatty fish (salmon, tuna), leafy greens, and berries can significantly impact arthritis symptoms. Reduce processed foods, red meat, and sugary drinks. Consult a registered dietitian for personalized dietary advice.
Mind-Body Techniques
Explore mind-body techniques such as yoga and tai chi. These practices can improve flexibility, reduce stress, and enhance pain management. Find a qualified instructor to guide you through proper form and techniques. Regular meditation may also prove beneficial in managing pain and improving overall well-being.
Acupuncture, a traditional Chinese medicine technique, may provide pain relief for some individuals. Research suggests potential benefits, but it’s vital to seek treatment from a licensed acupuncturist.
Remember, these alternatives should complement, not replace, your doctor’s recommended treatment plan. Always discuss any changes to your treatment plan with your physician.